A CASE OF PYREXIA UNDER EVLUATION WITH? DRUG INDUCED RASH
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box
A 66 year old lady came to casualty with complaints of fever on and off since 1 week, generalized body swelling since 1 week, decreased urine output since yesterday,SOB continuous since 2 days
She's a homemaker and she underwent a tubectomy 30 years ago and she was diagnosed with hypertension 6 years ago n was started on antihypertensive medications which she uses regularly since 5 years.she was apparently asymptomatic 1 week ago then she developed high grade intermittent fever and went to a RMP doctor for which she was treated with 2 pints NS on day 1 and again 3 pints NS on day 3 after which patient developed generalised body swelling and rashes all over the body which was erythematous macule with no specific pattern and again yesterday night and then she developed SOB since 2 days which was continuous in nature and present at rest.she doesn't have any similar complaints in the past.she complaints of decreased micturition since yesterday.there's no significant family history.
On examination patient is conscious, coherent and cooperative.
Patient has no pallor, icterus,cyanosis, clubbing,edema,lymphadenopathy
Vitals:
Temp-98.4 F
PR-88 BPM
RR-24 cpm
BP-140/80 mm Hg
Spo2-99%
GRBS-205 mg/dl
Systemic examination:
CVS- S1S2+, no murmurs heard
RS-NVBS+, BAE+
P/A- soft,NT
CNS-NFD
INVESTIGATONS:
Haemogram:
Hb-11 gm/dl
TLC-21,700
PLT-70,000
LFT:
Tb-3.69
Db-2.30
AST-30
ALT-38
ALP-513
TP-5.6
ALB-2.28
RFT:
Urea-67
Creatinine-3.8
Uric acid-7.3
Ca-10
Phosphate-2.0
Na+-135
K+ - 3.9
Cl- -98
Urinary electrolytes:
Spot Na-211
Pottasium- 10.5
Chloride-240
Clinical image of abdomen
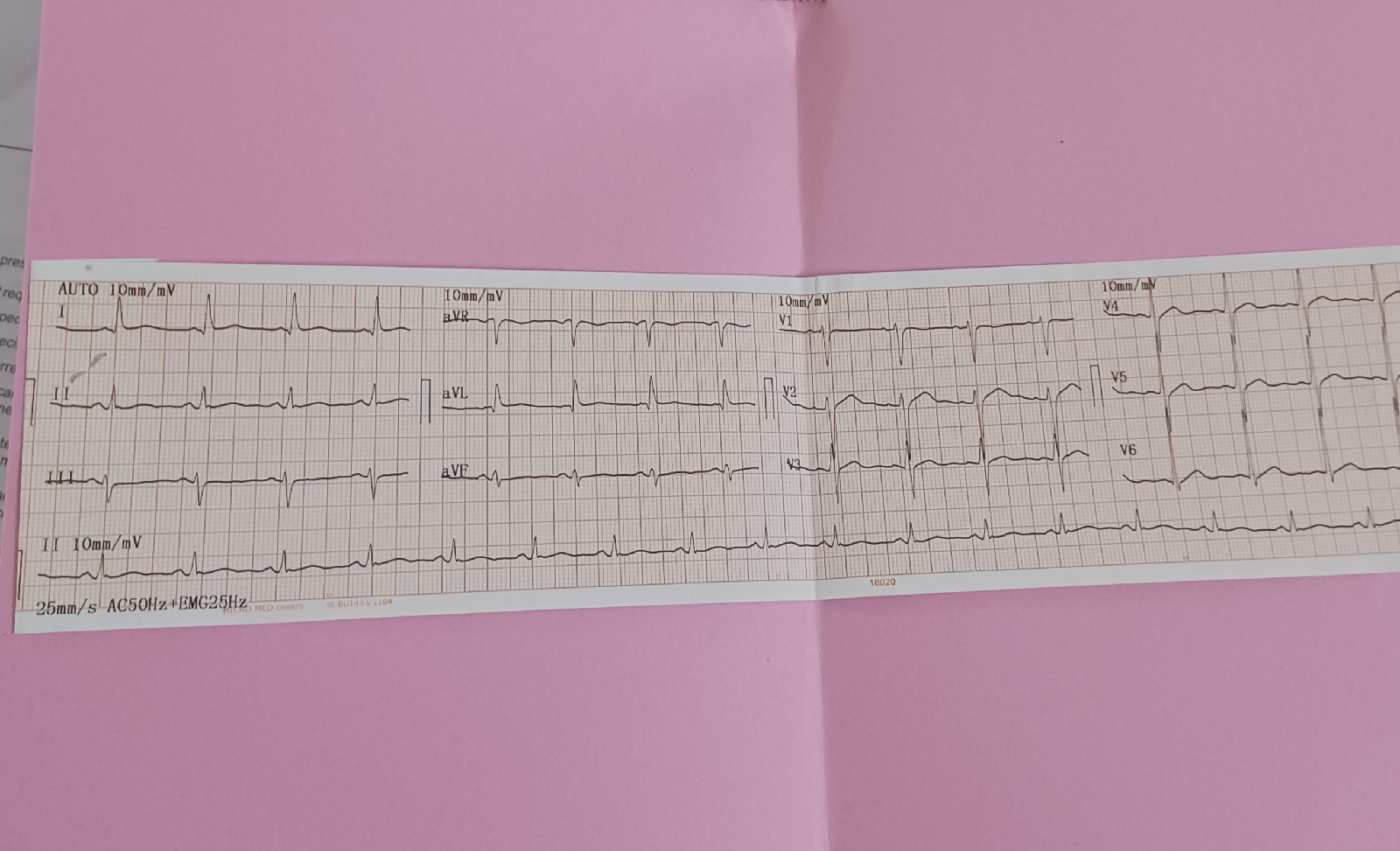
ECG:
-Raised echogenicity of b/l kidneys.correlate with RFT.
-altered echogenicity of liver.correlate with LFT
X RAY
SEPSIS WITH MODS,ALLERGIC INTERSTITIAL NEPHRITIS,
WITH DRUG INDUCED RASH
DENOVO DM 2
TREATMENT GIVEN:
1) INJ.LASIX 40 MG/IV/STAT
2)INJ.AVIL 1 AMP/IV/STAT
3)INJ.NEOMOL 1GM/IV/SOS IF TEMP >102 F
4)T.PCM 650 PO/TID
5)INJ.PIPTAZ 2.25 GM/IV/TID AFTER TEST DOSE WITH 4.5 GM/IV/STAT
6)OINT.LIQUID PARAFFIN FOR L/A BD
7)IVF NS @UO+75
SOAP NOTES
AMC BED NO 5
14/5/22
Day 7
S
Shortness of breath decreased
Pedal edema decreased
Rash decreased
O
Pt is C/C/C
No pallor,cyanosis,icterus ,clubbing,lympadenopathy,and
edema
Temp -96.6
Bp_120/70 mmHg
PR 82bpm
RR 20 cpm
GRBS 218mg/dl
Urine output 1000 ml
CNS _NAD
CVS S1 S2
No crepts
P/A_ tender at epigastric region
A
SEPSIS WITH MODS
ALLERGIC INTERSTITIAL NEPHRITIS
DRUG INDUCED RASH
DENOVO DM 2
P
1 INJ ACTRAPID INSULIN BD
2 INJ RANTAC 50 OD
3 INJ LASIX 20 IV BD
4 INJ AVIL 1 amp sos
5 TAB WYSOLONE 20 mg
6 TAB SEVALMER 800 mg
7 INJ NEOMOL 1gm IV SOS
If temp >102
8 Tab PCM 650 mg po TID
9 OINT LIQUID PARAFFIN for L/A BD
10 IV FLUIDS NS
11 Tab LEVOCETRIZNE 5mg po HS